While there are countless advancements in science for diabetes these days, mobile health tools (mHealth) have become increasingly popular for their ability to transform the way people visualize their blood glucose (BG) levels in real time – and without finger sticks. Current data shows that continuous glucose monitoring (CGM) technology, which is a type of wearable mobile health (mHealth) tool, may positively impact a wide variety of diabetes outcomes, including better management of BG levels, reduced complications, and overall improvements in quality of life. With more patients asking about these devices and applications, many healthcare professionals are taking steps toward increasing their knowledge of how CGM works and its pros and cons.
Managing Diabetes with mHealth Tools
Monitoring and managing BG levels helps to avoid health complications from diabetes, and mHealth tools offer a promising solution to enhance BG management.1 mHealth tools include any type of device or technology that a patient can engage with, typically in real time, in an effort to manage their health.2 Many tools are available for BG surveillance, which not only benefit the patient, but can guide the healthcare provider (HCP) in giving targeted advice and bridges the gap in communication between the patient and healthcare team. Although measurement of hemoglobin A1C is a valuable way to track BG over time, certain mHealth options allow tracking of daily changes in BG which can help identify opportunities to adjust meals, medications, and lifestyle habits to help keep BG in a healthy range.3,4
mHealth Uses and Considerations
CGM reduces the need for the traditional finger stick blood samples used to measure BG and improves reliability of BG readings.1 Although many of the mHealth devices are easy to use, education for both HCPs and patients on their use can help to ensure compliance.
Orgain’s Nutrition Advisor Laura Andromalos, MS, RD, CSOWN, CDCES, states “While CGMs significantly reduce finger sticks, it’s important to remind patients that finger sticks are still necessary for calibrating most devices or confirming readings that seem inaccurate. It’s part of managing expectations when transitioning to CGM.”
It’s also important that HCPs know how to set up a CGM system and interpret the results of their patients. According to Andromalos, “When reviewing CGM reports, there is a lot of data! It can be overwhelming for patients and clinicians. Upon downloading the report, there is a section titled ‘time in ranges’ that displays how many minutes the patient spends in their target range, as well as below and above it – this is a good place to focus. A goal of 70% “time in range” is common, although goals always must be individualized to your patient. If you’re supporting a patient to make changes to improve their time in range, start with the lows (low blood sugar). Hypoglycemia is typically more life-threatening than hyperglycemia. In the past, we only had A1C as our primary measure of glycemic management. With the development of CGM, we can use time in range to learn more about lows and highs on a daily basis versus just having an average blood sugar over three months with A1C.”
Most CGMs consist of 3 main parts:
- A monitor to display the information (this can be the smartphone using an app)
- A sensor/electrode is deposited on a needle that is inserted into the subcutaneous tissue of the patient
- A transmitter that sends the data to the monitor
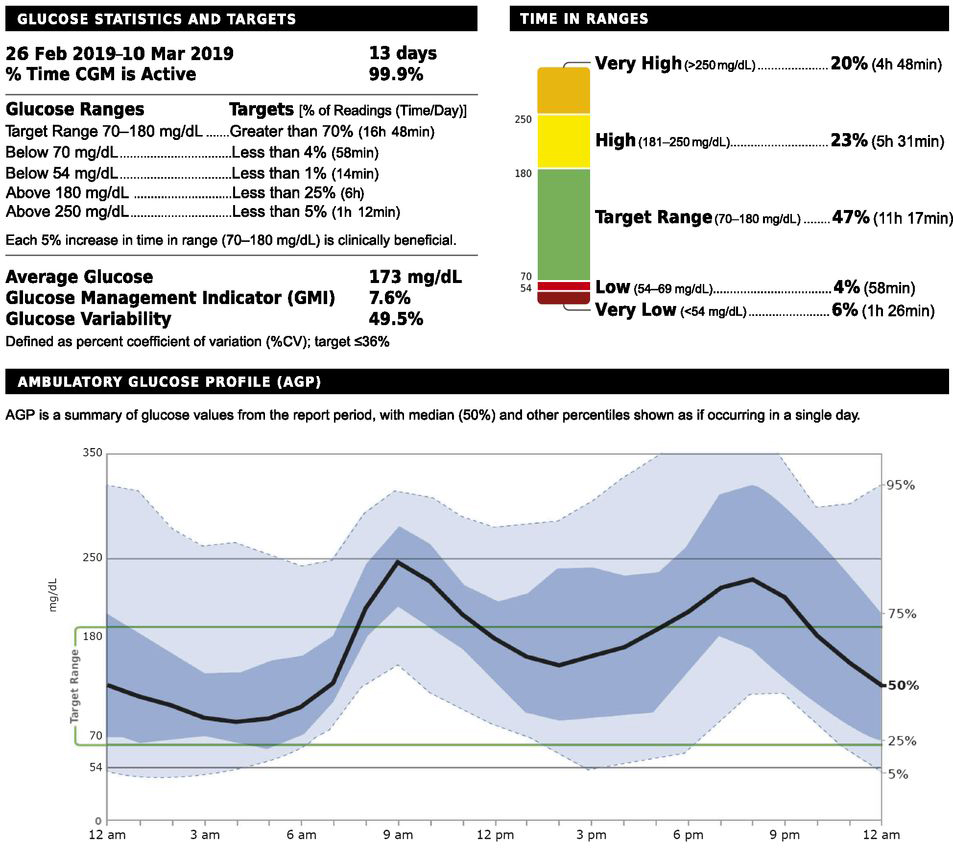
Many CGM models update the BG display every 1 to 5 minutes.1,3 To put the data output into perspective, see the CGM report below, which includes the “Time in Ranges” section:
A Review of Common CGM Technology – Monitors, Apps and Software
Continuous Glucose Monitors
Continuous glucose monitors (CGMs) provide ongoing surveillance and identification of high or low BG levels and offers a better understanding and awareness of lifestyle and habits, which can finetune diabetes management and prevent complications.7 In addition to the BG, some of these handy monitors allow patients to see trends and alerts right from their mobile device and all are accessible to HCPs in an effort to help patients better manage BG within acceptable ranges.2
A narrative review found that the use of continuous glucose monitors, along with diet and exercise, showed improvement in glycemic and weight control in individuals with type 2 diabetes who had been counseled on appropriate BG ranges.4
Smartphone Apps
A review of mHealth apps shows promise for their use in disease management. However, with the cost of the device and low health literacy being potential barriers for widespread use, innovative solutions are needed to educate vulnerable populations in an effort to make these devices accessible.6
Smartphone apps offer many different functions for tracking health. These apps can connect with a CGM, glucometer or use patient-entered data. These can include ways to track diet, activity, and medication, and provide a vehicle for feedback from HCPs.6 However, a surge in nonregulated apps points to a need for regulation, standardization, and quality control.7 In the meantime, patients can seek guidance from their HCP when choosing an app.
Software
Some patients and HCPs prefer to track and analyze data and communicate advice through a computer software system. CGM software allows for quick access to a variety of reports and can help patients and HCPs better understand and assess health-related insights and trends.
mHealth Tools Can Revolutionize Diabetes Management
Diabetes can be difficult to manage and typically requires self-monitoring, consistent communication with a healthcare team and a high level of health literacy.1 mHealth devices take the guesswork out of tracking BG and ultimately help patients and HCPs identify health habits leading to out-of-range BG readings and focus on safe and effective strategies to manage BG.1,7 This technology has revolutionized diabetes management and is becoming even more mainstream with companies such as Apple considering a non-invasive CGM feature built into an upcoming Apple Watch model. Although BG levels can be recorded with pen and paper, CGM captures ongoing, comprehensive changes that help patients and HCPs recommend lifestyle and medication habits for better BG management.2 With proper instruction for HCPs and patients on device capabilities, this technology can make tracking BG easier, more time efficient, and allow HCPs to provide targeted advice on BG management transforming diabetes care.6
Considerations in Counseling Patients on CGM
Identifying appropriate patients for CGM is crucial for the success of this BG monitoring format. To help better educate patients, healthcare professionals should not only review and understand the components of the selected device, app or software but familiarize themselves with CGM-specific vocabulary. Androlamos also offers this advice, “As diabetes clinicians, we can get excited and want to geek out about the amount of data that we can gather from our patient’s devices. Remember that there is a person behind the data! Your patient lived through those lows and highs and there may be emotions, such as fear or shame, connected to the numbers. Keep your counseling and education sessions patient-focused and use supportive language.” She recommends these helpful guidelines from The American Diabetes Association: The Use of Language in Diabetes Care and Education8
Resources
Please find below a list of popular apps and software used to track and help manage blood glucose. While this list is not inclusive of all technology, it offers a snapshot of some well-known options of which Orgain has no affiliation.
CGMs and Compatible Apps
- Freestyle Libre: Options include Freestyle Libre 2 and Freestyle Libre 14 Day sensors. Learn more about the system here.
- Dexcom G6: Learn more about the app here.
- Eversense: Learn more about the app here.
- Guardian Connect System: Learn more about the system and app here.
Smartphone Apps
- Glucose Buddy: Offers an option to self-test and manually log BG or connect to CGM.
- Health2Sync: Offers an option to self-test and manually log BG or syncs with BG meter to log BG.
- mySugr: Syncs with BG meter to log BG.
- OneTouch Reveal: Offers a variety of meters and apps that connect for BG logging.
- BeatO: Pairs with the BeatO glucometer. If using a different glucometer, manual logging is available.
Software
- Diabetes Partner: Track BG and lifestyle habits, analyze and send to HCP.
- Dexcom Clarity: Track data, analyze trends and share with HCP.
- SmartLog: View, analyze and share BG data.
![]()
1 Shan R, Sarkar S, Martin SS. Digital Health Technology and Mobile Devices for the Management of Diabetes Mellitus: State of the Art. Diabetologia 2019; 62(6):877-887. doi: 10.1007/s00125-019-4864-7.
2 University of Illinois Chicago. How to Use Mobile Technology to Manage Diabetes. Available at: https://healthinformatics.uic.edu/blog/how-to-use-mobile-technology-to-manage-diabetes/, accessed 10/14/2021.
3 Reddy N, Verma N, Dungan K. Monitoring Technologies – Continuous Glucose Monitoring, Mobile Technology, Biomarkers of Glycemic Control. Endotext 2020. Available at: https://www.ncbi.nlm.nih.gov/books/NBK279046/, accessed 10/14/2021
4 Taylor PJ, Thompson CH, Brinkworth GD. Effectiveness and Acceptability of Continuous Glucose Monitoring for Type 2 Diabetes Management: A Narrative Review. Journal of Diabetes Investigation 2018; 9(4):713-725. doi: 10.1111/jdi.12807.
5 Aminuddin HB, Jiao N, Jiang Y, Hong J, Wang W. Effectiveness of smartphone-based self-management interventions on self-efficacy, self-care activities, health-related quality of life and clinical outcomes in patients with type 2 diabetes: A systematic review and meta-analysis. International Journal of Nursing Studies 2021; (116)103286. doi.org/10.1016/j.ijnurstu.2019.02.003
6 Sneha S, Thalla S, Rischie I, Shahriar H. Health Internet Technology for Chronic Conditions: Review of Diabetes Management Apps. JMIR Diabetes 2021; 6(3):e17431). doi: 10.2196/17431
7 Cappon G, Vettoretti M, Sparacino G, Facchinetti A. Continuous Glucose Monitoring Sensors for Diabetes Management: A Review of Technologies and Applications. Diabetes & Metabolism Journal 2019; 43(4): 383–397. doi: 10.4093/dmj.2019.0121
8 Dickinson JK, Guzman SJ, Maryniuk MD, O’Brian CA, Kadohiro JK, et al. The Use of Language in Diabetes Care and Education. American Diabetes Association Diabetes Care 2017; 40(12): 1790-1799. https://doi.org/10.2337/dci17-0041



